
This document is intended to provide guidance for eye care practitioners in the management of myopia in clinical practice. Those who developed this guidance recognize that research is continually evolving, and thus the content provided herein has been informed by currently available scientific research and may be reviewed and updated periodically. Care has been taken to ensure the information provided is balanced and objective to enable practitioners to manage their patients holistically.
Managing Myopia: A Clinical Response to the Growing Epidemic has been created in collaboration with those listed below and is endorsed by the following organizations: American Optometric Association, Singapore Optometric Association, American Academy of Optometry, Johnson & Johnson Vision.
Authors
- Alex Nixon, OD, MS, FAAO
- Noel Brennan, PhD, MScOptom, FAAO
Contributors
- David Berntsen, OD, PhD, FAAO
- Kamlesh Chauhan, PhD, MCOptom
- Xu Cheng, MD, PhD, FAAO, MBA
- David Chong, D Optom, BSc Optom, MSc Clinical Optom
- Lori Grover, OD, PhD
- Koh Liang Hwee, BSc Optom (Hons) UK, PhD
- Chui Wen Juan, B Optom Hons, M Optom, PGCOT
- Chew Wai Kwong, BSc MCOptom
- Shirley Loh, B Optom, PGCOT
- Michael Mayers, OD, FAAO
- Jerry Neidigh, OD
- Erin Nilon, BS, MBA
- Andrew Pucker, OD, PhD, FAAO, FSLS, appointed by ASCO
- Kathryn Richdale, OD, PhD, FAAO, appointed by ASCO
- Tan Li Li, PhD, M MedSc (Optom), BOptom (Hons), FBCLA, FAAO
- Ken Tong, Bsc Optom
- Jeffrey Walline, OD, PhD
- May Zhang, MD, PhD
What is myopia?
Myopia1 is a chronic, progressive disease characterized by excessive eye elongation, risk of associated sight-threatening complications, and a negative-powered refractive error.
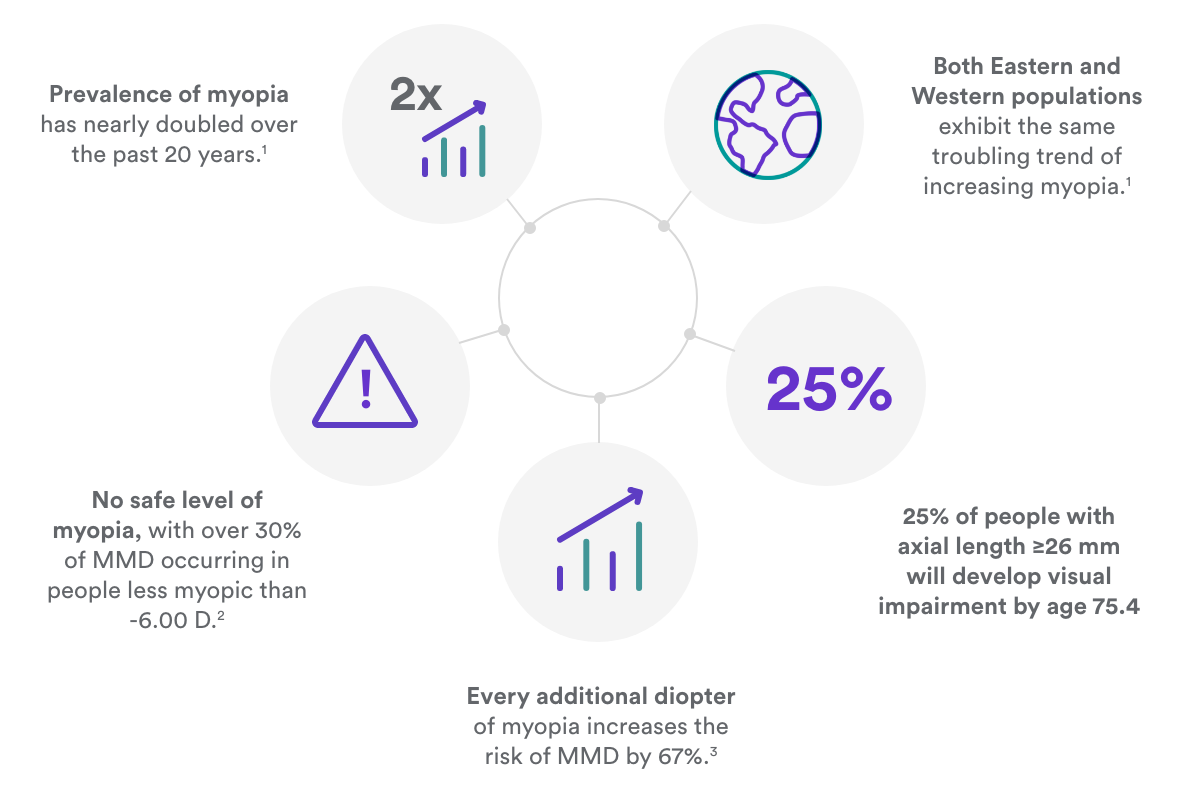
Growing global epidemic
- Reports of increased myopia prevalence in children first emerged in the 1980s2,3
- The prevalence has nearly doubled within the past 20 years in both eastern and western societies
- Prevalence among young adults is above 80% in many Asian regions,4 and 50% in the U.S. and parts of Europe5,6
- Children in the first wave of high myopia prevalence (those born after 1970) are now on the cusp of experiencing sight-threatening complications as adults
No safe level of myopia
- The elongated eye is susceptible to pathological complications with significant risks to eye health and vision
- Any degree of myopia increases the risk of sight-threatening complications, with some complications leading to blindness in adulthood7,8
- Each diopter increase in myopia results in 67% increased risk of myopic macular degeneration (MMD)9
Controlling myopia progression
- Eye care professionals now have the opportunity to slow myopia progression rather than just correct the visual symptoms
- Increased time outdoors can delay myopia’s onset10 and may slow its progression11
- Several myopia control therapies have shown efficacy of over 0.3 mm (around 0.75 D) over two to three years of treatment12-15
REFERENCES This guide addresses primary myopia rather than the secondary myopias, such as syndromic or cataract-related myopia, as defined in the IMI report. 1. Flitcroft DI et al. IMI–Defining and classifying myopia: a proposed set of standards for clinical and epidemiologic studies. Investigative ophthalmology & visual science. 2019;60:M20-30. 2. Lin LL et al. Nationwide survey of myopia among schoolchildren in Taiwan, 1986. Acta Ophthalmologica. 1988;66(S185):29-33. 3. Eong KA et al. Race, culture and myopia in 110,236 young Singaporean males. Singapore Med J. 1993 Feb 1;34(1):29-32. 4. Ding, Bo-Yuan, et al. "Myopia among schoolchildren in East Asia and Singapore." Survey of ophthal- mology 62.5 (2017): 677-697. 5. Vitale S et al. Prevalence of refractive error in the United States, 1999-2004. Arch Ophthalmol. 2008;126:1111-9. 6. Williams K et al. Increasing prevalence of myopia in Europe and the impact of education. Ophthalmology. 2015 Jul 1;122(7):1489-97. 7. Perkins ES. Morbidity from Myopia. Sight Sav Rev 1979;49:11-9. 8. Flitcroft DI. The Complex Interactions of Retinal, Optical and Environmental Factors in Myopia Aetiology. Prog Retin Eye Res 2012;31:622-60. 9. Bullimore MA, Brennan NA. Myopia Control: Why Each Diopter Matters. Optom Vis Sci 2019;96:463-5. 10. He M et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA. 2015;314:1142-8. 11. Wu PC et al. Myopia prevention and outdoor light intensity in a school-based cluster randomized trial. Ophthalmol. 2018;125:1239-50. 12. Chamberlain, Paul, et al. "A 3-year randomized clinical trial of MiSight lenses for myopia control." Optometry and Vision Science 96.8 (2019): 556-567. 13. Lam, Carly Siu Yin, et al. "Defocus Incorporated Multiple Segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial." British Journal of Ophthalmology 104.3 (2020): 363-368. 14. Chua, Wei-Han, et al. "At- ropine for the treatment of childhood myopia." Ophthalmology 113.12 (2006): 2285-2291. 15. Chen, Connie, Sin Wan Cheung, and Pauline Cho. "Myopia control using toric orthokeratology (TO-SEE study)." Investigative ophthalmology & visual science 54.10 (2013): 6510-6517.
Associated risks of myopia
Myopia is associated with increased risks to eye health in adulthood. These risks include:
- Myopic macular degeneration (MMD)1
- Staphyloma2
- Retinal detachment3
- Primary open-angle glaucoma4
- Cataracts5
Of these diseases, MMD and retinal detachment are the most devastating and have the strongest relationship to myopia and longer axial lengths (Table 1).6 Among people aged 75 years or older, cumulative risk of visual impairment (decimal VA 0.30 to 0.05 [approx. 20/60 to 20/400]) or blindness (decimal VA worse than 0.05 [20/400]) from all causes increases from 3.8% in eyes with an axial length less than 26 mm to 25% in eyes with an axial length of 26 mm or greater and more than 90% in eyes with an axial length of 30 mm or greater.7
Table 1: The increased likelihood (odds ratio) of a myopic person > 60 years developing eye disease versus an emmetrope by degree of myopia6
|
Degree of myopia |
|||
| -0.50 to -3.00 D | -3.00 to -6.00 D | -6.00 D or more myopic | |
|---|---|---|---|
| MMD | 13.6 | 73 | 73 |
|
Retinal detachment |
3.2 | 8.8 | 12.6 |
| Visual impairment† | 0.9 | 1.7 | 5.5* |
*Applies only to myopia of -6.00 to -10.00 D. Odds ratios are 7.8 for myopia of -10.00 to -15.00 D and 88 for myopia more than -15.00 D.
†Decimal visual acuity of 0.30 to 0.05 (approx 20/60 to 20/400).
REFERENCES 1. Ohno-Matsui K et al. Updates of Pathologic Myopia. Prog Retin Eye Res 2016;52:156-87. 2. Ohno-Matsui K, Jonas JB. Posterior staphyloma in pathologic myopia. Prog Retin Eye Res 2019;70:99-109. 3. Mitry D et al. The Epidemiology of Rhegmatogenous Retinal Detachment: Geographical Variation and Clinical Associations. Br J Ophthalmol 2010;94:678-84. 4. Marcus MW et al. Myopia as a Risk Factor for Open-Angle Glaucoma: A Systematic Review and Meta-Analysis. Ophthalmol 2011;118:1989-94. 5. Pan CW et al. Myopia and Age-Related Cataract: A Systematic Review and Meta-Analysis. American Journal of Ophthalmology 156.5 (2013): 1021-1033. 6. Haarman AE et al. The Complications of Myopia: A Review and Meta-Analysis. Investigative Ophthalmology & Visual Science. 2020 Apr 9;61:49. 7. Tideman JW et al. Association of axial length with risk of uncorrectable visual impairment for Europeans with myopia. JAMA Ophthalmol 2016;134:1355-63.
Myopia is the biggest threat to eye health of the 21st century
Eye care professionals should embrace new therapies treating children as soon as signs of myopia appear in order to reduce the risk of sight-threatening complications in later life.
REFERENCES 1. Holden BA et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmol 2016;123:1036-42. 2. Wong, Yee-Ling, et al. "Prevalence, risk factors, and impact of myopic macular degeneration on visual impairment and functioning among adults in Singapore." Investigative Ophthalmology & Visual Science 59.11 (2018): 4603-4613. 3. Bullimore MA, Brennan NA. Myopia Control: Why Each Diopter Matters. Optom Vis Sci 2019;96:463-5. 4. Tideman JW et al. Association of axial length with risk of uncorrectable visual impairment for Europeans with myopia. JAMA Ophthalmol 2016;134:1355-63.
Managing myopia in children: the need for a new approach
Myopia is a continuum of disease stages which should be assessed as early as possible. Myopia may continue to progress beyond the teenage years1 and the associated disease risk increases exponentially with severity of myopia,2,3 making early diagnosis and treatment crucial to lifetime eye health.
Early myopia onset increases risk of high myopia
Myopia progresses more quickly in younger children.4 Because early onset implies more years of progression, myopes younger than 12 are at greater risk of developing high myopia. This is why it’s essential to:
- Examine children at least once between the ages of 3-5 years to establish baseline measurements
- Examine all children at least annually until they reach 18 years old
Table 2: Classification of myopia by spherical equivalent refractive error5
| Emmetropia (Pre-Myopia if ≤ age 12)6 | Myopia6,7 |
High Myopia7 |
|
| Refractive error | +0.75 to -0.49 D | -0.50 to -4.99 D | -5.00 D and more myopic |
Refractive error predicts myopia onset
Numerous risk factors can help predict myopia onset, but the best predictor is cycloplegic spherical equivalent refractive error at a given age. A child with low hypermetropic refraction for a given age (Table 3) has greater than an 80% likelihood of myopia onset by age 13.5 This approach provides a simple clinical method to evaluate risk of myopia onset that is just as accurate as more complex algorithms.
Table 3: Cycloplegic spherical equivalent autorefraction threshold by age, for children at high risk of becoming myopic by 8th grade
|
Age |
6 |
7-8 |
9-10 |
11 |
| Refractive error |
< +0.75 D |
≤ +0.50 D |
≤ +0.25 D |
≤ +0.00 D |
REFERENCES 1. Pärssinen, Olavi, and Markku Kauppinen. "Risk factors for high myopia: a 22-year follow-up study from childhood to adulthood." Acta Ophthalmologica 97.5 (2019): 510-518. 2. Bullimore MA, Brennan NA. Myopia Control: Why Each Diopter Matters. Optom Vis Sci 2019;96:463-5. 3. Haarman AE et al. The complications of Myopia: A review and Meta-Analysis. Investigative Opthalmology & Visual Science 2020 Apr 9;61:49. 4. Chua SY et al. Age of Onset of Myopia Predicts Risk of High Myopia in Later Childhood in Myopic Singapore Children. Opthal Physiol Opt 2016;36:388-94. 5. World Health Organization - Brien Holden Vision Institute. The impact of myopia. In: The Impact of Myopia and High Myopia. Report of the Joint World Health Organization--Brien Holden Vision Institute Global Scientific Meeting on Myopia. Available at: https://www.visionuk.org.uk/download/WHO_Report_Myopia_2016.pdf. 6. Flitcroft DI et al. IMI–Defining and classi- fying myopia: a proposed set of standards for clinical and epidemiologic studies. Investigative ophthalmology & visual science. 2019;60:M20-30. 7. World Health Organization - Brien Holden Vision Institute. The impact of myopia. In: The Impact of Myopia and High Myopia. Report of the Joint World Health Organization-Brien Holden Vision Institute Global Scientific Meeting on Myopia. Available at: https://www.visionuk.org.uk/download/WHO_Report_Myopia_2016.pdf. 8. Zadnik K et al. Prediction of Juvenile Onset Myopia. JAMA Opthalmol 2015;133:683-9.
Deciding when and how to treat myopia
Importance of early treatment: every diopter matters
- Progression is highly likely once a child is identified as pre-myopic or myopic.1 The goal of myopia control is to restrict axial length and refraction as much as possible but certainly to keep axial length below 26 mm2,3 and less than 5 D of myopia.4
- Reducing myopia by 1.00 D reduces the likelihood of a patient developing myopic macular degeneration by about 40%5
- Begin clinical treatment for all myopic children 12 years of age or less and offer lifestyle guidance at a minimum for pre-myopic children
Risk factors for myopia
- Younger age6
- Refractive error (see Table 3)7
- Minimal time outdoors (< 2 hrs/day)8
- Near work for longer duration or at a shorter working distance9,10
- Myopic parents11
Lifestyle guidance
One evidence-based method to delay the onset of myopia in children is spending time outdoors.12 Growing evidence supports that more time outdoors may also slow the progression of myopia.13 Increased outdoor time may benefit all children.
Table 4: Likelihood of myopia progression or onset and recommended clinical action by age and refractive status
|
Refractive status |
Pre-myopia (≤ 12 yrs) |
Myopia (≤ 12 yrs) |
Myopia (13+ yrs) |
|
Probability |
Myopia onset highly likely |
Progression highly likely |
Progression possible |
|
Clinical action† |
Close monitoring‡ |
Myopia control highly recommended |
Present myopia control |
†Lifestyle guidance is a suggested component of all myopia control therapy.
‡Treatment of pre-myopia is at the discretion of the parent/patient and clinician.
REFERENCES 1. Mutti DO et al. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Invest Ophthalmol Vis Sci. 2007;48:2510-9. 2. Haarman AE et al. The Complications of Myopia: A Review and Meta-Analysis. Investigative Ophthalmology & Visual Science. 2020 Apr 9;61:49. 3. Tideman JW et al. Association of axial length with risk of uncorrectable visual impairment for Europeans with myopia. JAMA Ophthalmol 2016;134:1355-63. 4. World Health Organization–Brien Holden Vision Institute. The impact of myopia. In: The Impact of Myopia and High Myopia. Report of the Joint World Health Organization–Brien Holden Vision Institute Global Scientific Meeting on Myopia. Available at: https://www.visionuk.org.uk/download/WHO_Report_Myopia_2016.pdf. 5. Bullimore MA, Brennan NA. Myopia Control: Why Each Diopter Matters. Optom Vis Sci 2019;96:463-5. 6. Chua SY et al. Age of Onset of Myopia Predicts Risk of High Myopia in Later Childhood in Myopic Singapore Children. Ophthal Physiol Opt 2016;36:388-94. 7. Zadnik K et al. Prediction of Juvenile-Onset Myopia. JAMA Ophthalmol 2015;133:683-9. 8. Wu PC et al. Increased Time Outdoors Is Followed by Reversal of the Long-Term Trend to Reduced Visual Acuity in Taiwan Primary School Students. Ophthalmology. 2020 Feb 8:S0161-6420(20)30139-1. 9. Huang et al. The Association between Near Work Activities and Myopia in Children: A Systematic Review and Meta-Analysis. PLoS One 2015;10:e0140419. 10. Wen L et al. Objectively measured near work, outdoor exposure and myopia in children. British Journal of Ophthalmology Published Online First: 19 February 2020. doi: 10.1136/bjophthalmol-2019-315258. 11. Tedja MS et al. IMI - Myopia Genetics Report. Invest Ophthalmol Vis Sci 2019;60:M89-M105. 12. He M et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA. 2015;314:1142-8. 13. Wu PC et al. Myopia prevention and outdoor light intensity in a school-based cluster randomized trial. Ophthalmol. 2018;125:1239-50.
Evaluating pre-myopia and myopia
Refractive error
- Primary method for diagnosing myopia and a routine measurement in every comprehensive eye examination1
- Accuracy and repeatability improve with use of cycloplegia and objective measurements (autorefraction)2
- Strongly correlated with axial length,3 but substantially less repeatable than optical biometry even with cycloplegia4,5
- Misleading interpretation can occur with orthokeratology and/or atropine
Axial length (optical biometry)
- Primary metric for monitoring eye elongation
- Highly repeatable measurement
- Relates directly to the pathological processes in myopia
- Doesn’t require cycloplegia
- Less susceptible to changes in the anterior optics of the eye which may occur over the course of treatment such as orthokeratology or atropine therapy
Key points for monitoring
- Young myopes will progress, so set this as the expectation6
- Average treatment efficacy can be referenced from randomized clinical trials
- Monitor myopia control therapy use, acceptance, and maintenance every six months
- Evaluate progression using at least one (1) year of data to avoid seasonal changes and reduce measurement noise (even with optical biometry)
- Treatment efficacy cannot be determined for an individual patient because there is no way to know how that individual would have progressed if left untreated
- Refer to population-based normative data to assess progression (see Table 5)
REFERENCES 1. American Optometric Association, Comprehensive Pediatric Eye and Vision Examination. https://www.aoa.org/AOA/Documents/Practice%20Management/Clinical%20Guidelines/EBO%20 Guidelines/Comprehensive%20Pediatric%20Eye%20and%20Vision%20Exam.pdf, accessed September 3, 2020. 2. Morgan, Ian G., et al. Cycloplegic refraction is the gold standard for epidemiological studies. Acta Ophthalmologica 93.6 (2015): 581-585. 3. Hou, Wei, et al. Axial elongation in myopic children and its association with myopia progression in the Correction of Myopia Evaluation Trial (COMET). Eye & contact lens 44.4 (2018): 248. 4. Buckhurst, Phillip Jonathan, et al. "A new optical low coherence reflectometry device for ocular biometry in cataract patients." British Journal of Ophthalmology 93.7 (2009): 949-953. 5. Bullimore, Mark A.et al. "The repeatability of automated and clinician refraction." Optometry and Vision Science: Official Publication of the American Academy of Optometry 75.8 (1998): 617-622. 6. Donovan L et al. Myopia progression rates in urban children wearing single-vision spectacles. Optom Vis Sci 2012;89:27-32.
Monitoring and efficacy
Expected progression without myopia control
Eye growth should be expected in all young patients, with even stable emmetropic eyes growing around 0.1 mm per year from age 6 to 14.1 Younger myopes will progress faster on average, with average rate of progression in 7-year-old children nearly double that of 11-year-old children.2 Individual progression near the mean values by age in Table 5 should not be considered normal or healthy, since any myopia progression will exponentially increase associated disease risk. Individual progression rates vary considerably across the population.3
Caution with myopia control calculators
Myopia control calculators offer reasonable estimates of normal progression without myopia control therapy. The calculated myopia control effect, however, extrapolates a few years treatment effect for up to 11 years, omitting that treatment effect decreases over time and misleading users with overly optimistic treatment expectations.4
Communicating myopia control efficacy
While “percentage treatment” effect is easy to understand, it leads to inconsistent representation across the progression range and fails to capture that myopia control efficacy slows over time. Myopia control treatment effect tends to be more of an absolute effect than a proportional effect.4 The best descriptor of myopia control efficacy is the cumulative absolute reduction in elongation or refractive error (e.g., total mm or D).
Table 5: Mean progression for myopic Asians and non-Asians by axial length and refractive error across age2,5
| Age | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|
| Axial length (mm) | Asian | 0.52 | 0.46 | 0.41 | 0.36 | 0.32 | 0.28 |
| Non-Asian | 0.35 | 0.31 | 0.28 | 0.25 | 0.22 | 0.20 | |
| Refractive error (D) | Asian | -1.12 | -0.94 | -0.78 | -0.66 | -0.56 | -0.50 |
| Non-Asian | -0.98 | -0.82 | -0.69 | -0.56 | -0.45 | -0.35 |
REFERENCES 1. Mutti DO, Hayes JR, Mitchell GL et al. Refractive Error, Axial Length, and Relative Peripheral Refractive Error before and after the Onset of Myopia. Invest Ophthalmol Vis Sci 2007;48:2510- 9. 2. Donovan L et al. Myopia progression rates in urban children wearing single-vision spectacles. Optom Vis Sci 2012;89:27-32. 3. Chua SY et al. Age of Onset of Myopia Predicts Risk of High Myopia in Later Childhood in Myopic Singapore Children. Ophthal Physiol Opt 2016;36:388-94. 4. Brennan NA, Cheng X. Commonly Held Beliefs About Myopia That Lack a Robust Evidence Base. Eye Contact Lens 2019;45:215-25. 5. Brennan NA et al. Influence of Age and Race on Axial Elongation in Myopic Children. Optom Vis Sci 2018; 95: eAbstract 180072.
Average myopia control treatment effect
Numerous clinical studies provide cumulative myopia control effect for individual therapies in millimeters or diopters over a 2 to 3-year period, with multiple studies providing evidence of a 0.30 mm reduction in elongation (about 0.75 D).1-4 Since the maximum effect observed to date is 0.44 mm (about 1.00 D) over a 7-year period,5 treatment should begin as early as possible. Combination therapy may enhance myopia control efficacy compared to a single treatment.6
Monitoring
Myopia control therapy use, acceptance, and maintenance should be frequently monitored following treatment initiation or modification and at least every six (6) months once treatment is established. Frequent monitoring helps reduce barriers to use, identify non-compliant or risky behaviors, and address any problems as early as possible, supporting safe and consistent use of the myopia control therapy. Axial length and cycloplegic refractive error may be measured at frequent intervals, but should be evaluated over at least one year before considering therapeutic changes or supplemental therapy because progression can vary seasonally.7 Knowing efficacy is similar across treatments, it is most critical that the treatment regimen fits the patient’s lifestyle, expectations, motivation, and their abilities.
Stopping treatment
Once myopia control treatment has begun, myopia stabilization cannot be differentiated from an effective myopia control therapy. Because there is evidence for progression in some adults,8 myopia control can be continued beyond the teenage years if the treatment is well accepted. If not well accepted, an alternative myopia control therapy can be considered. Rebound after myopia control discontinuation may occur and regular monitoring should be continued after stopping therapy.
Sample myopia monitoring schedule
Interim(6 months)
- Focused history including at a minimum:
- Care and maintenance of therapy
- Frequency and usage of therapy
- Patient acceptance and satisfaction with therapy
- Visual acuity
- Binocular vision and accommodation (can be impacted by myopia control therapy)
- Measure axial length (if possible) and refractive error
- Assess therapy-related ocular health
- Additional testing as indicated by myopia control therapy
Annual (12 months)
- Comprehensive eye exam (w/cycloplegic refractive error if possible)
- Review myopia control therapy (as described above)
- Measure axial length (if possible)
- Review progression and compare to personalized goals
REFERENCES 1. Chamberlain, Paul, et al. "A 3-year randomized clinical trial of MiSight lenses for myopia control." Optometry and Vision Science 96.8 (2019): 556-567. 2. Lam, Carly Siu Yin, et al. "Defocus Incorporated Multiple Segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial." British Journal of Ophthalmology 104.3 (2020): 363-368. 3. Chua, Wei-Han, et al. "Atropine for the treatment of childhood myopia." Ophthalmology 113.12 (2006): 2285-2291. 4. Chen, Connie et al. "Myopia control using toric orthokeratology (TO-SEE study)." Investigative Ophthalmology & Visual Science 54.10 (2013): 6510-6517. 5. Santodomingo-Rubido et al. Long-Term Efficacy of Orthokeratology Contact Lens Wear in Controlling the Progression of Childhood Myopia. Curr Eye Res 2017;42:713-20. 6. Kinoshita et al. Efficacy of combined orthokeratology and 0.01% atropine solution for slowing axial elongation in children with myopia: a 2-year randomised trial. Sci Rep 10, 12750 (2020). 7. Gwiazda, Jane, et al. Seasonal variations in the progression of myopia in children enrolled in the correction of myopia evalua- tion trial. Investigative Ophthalmology & Visual Science 55.2 (2014): 752-758. 8. Pärssinen O, Kauppinen M. Risk factors for high myopia: a 22-year follow-up study from childhood to adulthood. Acta Ophthalmol. 2019;97:510-8.
Personalizing myopia control therapy
Treatments described here have been investigated in clinical studies for their safety and effectiveness. Efficacy and performance may vary significantly between products (e.g., for different brands) and it is important to note that some treatments are currently prescribed off-label. Choosing the right one will depend on the individual patient's lifestyle, age, maturity, and refractive error. This diagram can be helpful in guiding your conversation with patients and their parents.

REFERENCES 1. Santodomingo-Rubido, Jacinto, et al. Myopia control with orthokeratology contact lenses in Spain: a comparison of vision-related quality-of-life measures between orthokeratology contact lenses and single-vision spectacles. Eye & Contact Lens 39.2 (2013): 153-157. 2. Rah, Marjorie J et al. Vision specific quality of life of pediatric contact lens wearers. Optometry and Vision Science 87.8 (2010): 560-566. 3. Walline, Jeffrey J et al. Contact Lenses in Pediatrics (CLIP) Study: chair time and ocular health. Optometry and Vision Science 84.9 (2007): 896-902. 4. Bullimore MA. The Safety of Soft Contact Lenses in Children. Optom Vis Sci 2017;94(6):638-646. doi:10.1097/ OPX.0000000000001078. 5. Yam, Jason C., et al. Two- year clinical trial of the low-concentration atropine for myopia progression (lamp) study: phase 2 report. Oph- thalmology 127.7 (2020): 910-919. 6. Kinoshita, Nozomi et al. efficacy of combined orthokeratology and 0.01% atropine solution for slowing axial elongation in children with myopia: a 2-year randomised trial. Scientific Reports 10.1 (2020): 1-11.
Appendix: managing myopia in children into early adulthood: quick guidelines
Comprehensive eye examination1
Care Process Includes:
- Visual acuity (OD/OS/OU Distance and Near)
- Objective and subjective refraction (with cycloplegia if possible)
- Binocular vision, ocular motility, and accommodation
- Color vision
- Pupil response
- Intraocular pressure
- Ocular anterior segment and adnexa
- Ocular posterior segment (internal eye)
- Supplemental testing as indicated based on clinical expertise
Identify children who have myopia or are at risk of myopia onset and discuss:
- Eye diseases associated with myopia
- Benefits of time outdoors
- Concept of myopia control therapy versus traditional vision correction
- The need for myopia control consultation and/or treatment initiation
Myopia control consultation, treatment and monitoring
Consultation
- Perform baseline measurements as appropriate (e.g. refractive error, corneal topography, and axial length)
- Present personalized options for myopia control (if applicable) based on motivation, lifestyle, and ocular characteristics
- Discuss available treatment, expectations, potential adverse effects, and review consent for treatment
- Collaborate with parent to set goals, address potential barriers, and create an action plan
Treatment
- Train both child and parent to apply, remove, disinfect and care for the treatment (as applicable)
- Prescribe wearing schedule
- Provide emergency contact number, if applicable
Monitoring
- Monitor myopia control therapy use, acceptance, and maintenance frequently following treatment initiation and at least every six (6) months
- Evaluate progression using at least one (1) year of data to avoid seasonal changes and reduce measurement noise
- Treatment efficacy cannot be calculated for an individual patient because there is no way to know how an individual’s myopia would have progressed untreated
REFERENCES 1. American Optometric Association, Comprehensive Pediatric Eye and Vision Examination. https://www.aoa.org/AOA/Documents/Practice%20Management/Clinical%20Guidelines/EBO%20Guidelines/Comprehensive%20Pediatric%20Eye%20and%20Vision%20Exam.pdf, accessed September 3, 2020.




